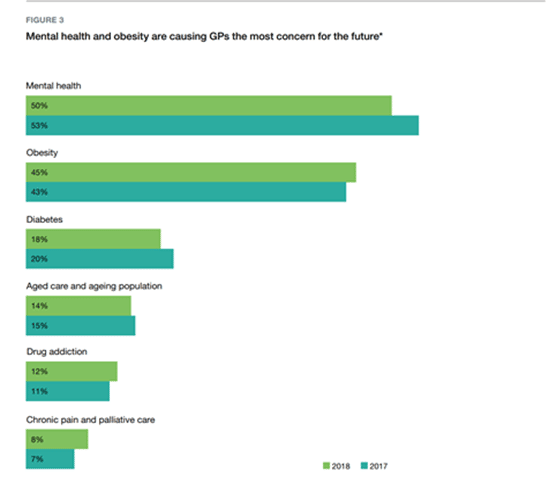
It comes as no surprise that in the recently published The General Practice: Health of the Nation report, mental health and obesity are causing GPs the most concern for the future:
Bariatric metabolic surgery appears to uniquely interrupt the weight-preserving cascade and allows patients to successfully adhere to the dietary and lifestyle modifications needed to attain long-term weight loss. It is currently the only intervention shown to consistently achieve substantial long-term weight loss for individuals with moderate to severe obesity (BMI above 35).
Health professionals are faced each day with patients who suffer from the consequences of excess weight. Until recently, there was little to offer in terms of practical and effective long-term solutions. Fortunately, the horizon now looks much brighter. As healthcare providers, we are uniquely positioned to identify and support these patients by starting a conversation about bariatric metabolic surgery and busting some myths to remove barriers to treatment.
MYTH: Diet and Exercise is all that people need to lose weight
REALITY:
- Once obesity grabs hold, it becomes exceedingly uncommon to escape its chokehold.
- While diet and exercise always serve to improve a patient’s overall health, they very rarely result in substantial long-term weight loss in patients with moderate to severe forms of obesity (BMI ≥35 kg/m2).
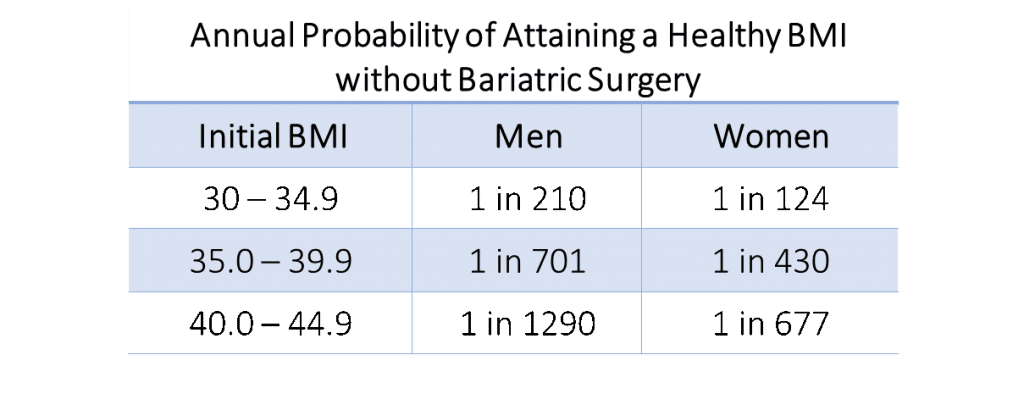
- A 10 year longitudinal study of 300,000 patients by the Department of Primary Care and Public Health Sciences, King’s College London, UK revealed the likelihood of a person at various BMIs attaining a healthy BMI within 12 months without bariatric metabolic surgery.
There is now consensus from over 50 leading professional organizations worldwide that bariatric surgery should be strongly considered for treatment of moderate-severe obesity and/or certain obesity-related comorbidities, such as type 2 diabetes mellitus.
MYTH: Most patients regain all of the weight they lost post-surgery.
REALITY: People achieve maximum weight loss 12-18 months after surgery. The
overwhelming majority (two-thirds or more depending on the procedure) maintain substantial weight loss for life. Bariatric surgery does not cure obesity, it puts it into remission. It requires lifelong adherence to nutritional recommendations and
behavioural changes for patients to maintain their successful outcomes long term.
MYTH: After bariatric surgery, patients will never eat “normally” again.
REALITY: People are concerned that they will constantly be hungry after surgery and yet unable to eat. In fact, bariatric metabolic surgery reduces the production of hunger hormones and causes a significant loss of hunger for most people. Immediately following surgery, there is a six week modified texture protocol to allow the new anatomy to heal, but after that they are able to eat small, healthy portions of most foods.
MYTH: Most patients suffer from severe diarrhea, nausea & vomiting after surgery.
REALITY:
It is an enduring misconception that after bariatric metabolic surgery people commonly suffer from severe diarrhea, nausea, and vomiting. The reality is that diarrhea is a relatively uncommon with constipation being far more typical due to inadequate fibre and fluid intake. It is important to perform a gastroscopy preoperatively with duodenal biopsies and disaccharidases assay to detect underlying conditions that may create loose bowels with certain food choices, such as coeliac disease or lactase, sucrase or maltase deficiency. This facilitates dietary modification after surgery should loose stools develop. Occasional bouts of nausea are sometimes seen in the early weeks and months following surgery. These episodes are usually related to inappropriate eating behaviours (eating too much, or too quickly) or food selection. They are easily remedied with dietary counselling, which is one of the many reasons dietitians are invaluable member of the treating team. It is also one of the reasons why it is important that dietitians are trained about the anatomical changes that occur in each procedure type, and how this impact on dietetic management.
MYTH: Most patients experience significant mineral & vitamin deficiencies.
REALITY: Daily vitamin supplements are required for each person after bariatric surgery. This is most easily achieved with a bariatric surgery specific multivitamin, rather than having to use a combination of regular vitamins. However, studies have shown that a substantial percentage of people (varying from 30-80% depending on the study and vitamin tested) with obesity have significant vitamin and mineral deficiencies BEFORE they undergo surgery. It is not surprising that some people require some degree of additional supplementation after surgery (e.g. Vit D, calcium citrate, iron, Vit B12 etc). Remember though, these vitamins are a supplement to a nutritious diet and not a replacement for one. This is also why it is important to check nutritional profiles before surgery, correct and monitor 3 monthly until normal levels are achieved and maintained before extending the testing interval to annually.
MYTH: Bariatric surgery is associated with a high morbidity & mortality rate.
REALITY: Surgeries are performed laparoscopically, significantly reducing morbidity and recovery time. The risk of mortality associated with laparoscopic bariatric surgery is extremely low and comparable to that of laparoscopic gallbladder surgery. The Australian Bariatric Surgery Registry monitors the safety and efficacy of bariatric surgeons, surgeries and devices. It reports a six-year mortality rate of 0.09% for death from ALL causes whether related to surgery or not, with around a third of those deaths having been shown to be unrelated to the procedure. The risk of significant non-life-threatening complications within 90 days of surgery is less than 3%. Overall, the risks associated with bariatric metabolic surgery tend to be greatly outweighed by the benefits of long-term weight loss and the resolution of weight-related health problems.
Dr Nova Jordaan is a medical doctor trained in Obesity Medicine. She has spent
nearly a decade managing the medical needs of weight loss surgery patients
before and after surgery to enhance the safety and outcomes of the procedures.
After attaining her medical degree at the University of Sydney she undertook further
training in Obesity Medicine at Harvard Medical School. She practices both medical and surgical obesity management at the Surgical Weight Loss Centre, Gold Coast and offers a complimentary, confidential initial consultation for people wanting to discuss their weight loss options.