Bariatric surgery has been shown to be particularly effective as a treatment for Type 2 Diabetes, sleep apnoea, infertility and highly effective at reducing cardiovascular risk.
Surgical technique has advanced significantly over the past 20 years, with bariatric surgeries now almost exclusively performed as laparoscopic operations with a lower morbidity profile than in the ‘open surgery’ era.
Referral to a surgical weight loss centre has been adopted in key management guidelines, which advise that:
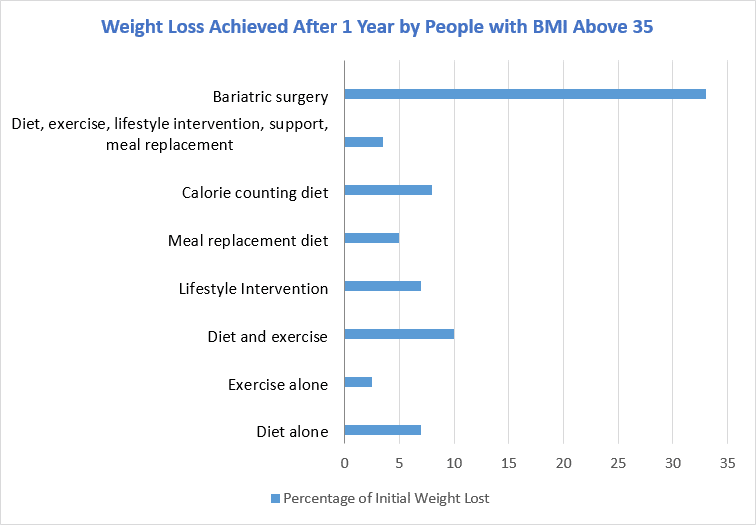
Bariatric surgery is currently the most effective intervention for severe obesity.
In 2013, the National Health and Medical Research Council (NHMRC) published the Clinical Practice Guidelines for the Management of Overweight and Obesity in Adolescents, Children and Adults in Australia, which may be taken into account in future litigation cases.
In essence, the NHMRC guidelines advise GPs to conduct the five A’s:
- ASK about, and
- ASSESS weight, along with readiness for behavioural change
- ADVISE about the health benefits of lifestyle change and weight loss
- ASSIST through lifestyle interventions, including:
- Reduced energy intake aiming for 2500 daily kilojoule deficit
- Increase physical activity to 5 hours weekly of moderate intensity exercise or 2.5 hours of vigorous activity
- Implement measures to support behavioural change
- Set a goal of at least 5% weight loss and review patients fortnightly for the first 3 months and continuing monitoring for at least 12 months. If there is less than 1% body weight reduction or no change in waist circumference after 3 months of active management, initiate additional interventions.
- ARRANGE an appropriate weight loss program
- For adults with BMI > 30 kg/m2 with poorly controlled Type 2 Diabetes and increased cardiovascular risk
- For adults with BMI > 35 kg/m2 and obesity related health complications
- For adults with BMI > 40 kg/m2, regardless of health
This sounds simple enough, but for many doctors it is not easy to initiate a conversation about weight issues with a patient. The major indemnity insurer, Avant, suggests that GPs fostering a trusting doctor-patient relationship is the key to successfully raising and managing this difficult issue in a sensitive manner. It is also recommended that weight, height, hip and waist measurements become a regular part of the consultation routine as a good way of initiating a conversation and making these discussions less uncomfortable.