Obesity has overtaken smoking as the leading cause of preventable disease and premature death in Australia.
It is therefore important to be able to easily identify people who are most likely to have obesity.
Once identified, people in this group can be further assessed to determine if and how they would benefit from having their obesity treated.
The World Health Organisation (WHO) defines obesity by the percentage body fat, over 25% for men and over 35% for women.
What does that mean in laymans terms? If more than a quarter of a man’s body if made up of fat, then he has obesity. If more than a third (roughly) of a women’s body is made up of fat, then she has obesity.
How do we identify people with obesity?
A good screening tool to identify people with obesity would be
- Quick
- Easy
- Non-invasive
- Free
- Based on information that most people already know or can easily find out without needing difficult or expensive equipment
- A reliable indicator of actually having obesity to maintains public trust in the result
- That is, it would be best if most of the people identified by the screening tool would turn out to actually have obesity on further testing and relatively few people are incorrectly categorised as having obesity.
BMI meets all of these criteria.
BMI = weight in kilograms
Height in metres x height in metres
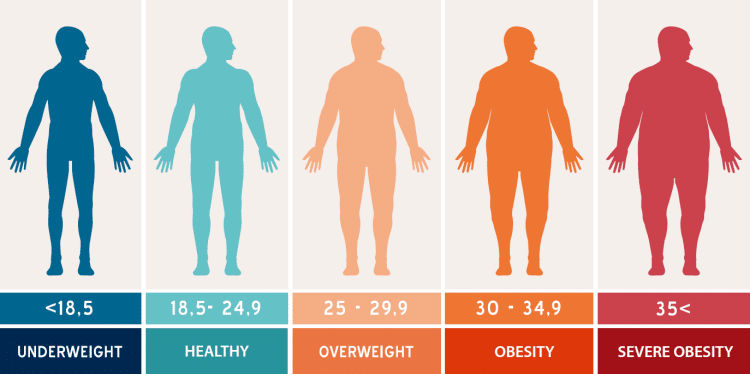
Large studies of people in the USA representing men and women of many ages and ethnic backgrounds show that having a BMI over 30 is highly predictive for having obesity as defined by the WHO (around 99% predictive for women and 95% predictive for men).
So if your BMI is above 30 it’s a good trigger to indicate that you may benefit from further assessment to see how your health is being impacted by obesity.
The most effective treatment for obesity is bariatric surgery. To identify if surgery is a suitable option, a BMI above 30 is used as a starting point for a full health assessment. If that person also has Type 2 diabetes and increased cardiovascular risk, Australian guidelines recommend bariatric surgery.
As BMI increases so does percentage body fat, and so does the impact of obesity on a person’s health.
A person with a BMI above 35 who suffers from obesity related health problems such as diabetes, sleep apnoea, infertility, PCOS, high blood pressure, cholesterol problems, heart disease, arthritis, stress urinary incontinence, fatty liver, migraines, depression and so forth, would also meet the Australian criteria for bariatric surgery.
A person with a BMI above 40, regardless of their current health status, would be eligible for bariatric surgery to reduce their risk of obesity related health problems and premature death.
What are the limitations of BMI?
BMI was first described by Adolphus Quetelet in the mid 19th century based on the observation that body weight was proportional to the square of the height in adults with normal body frame.
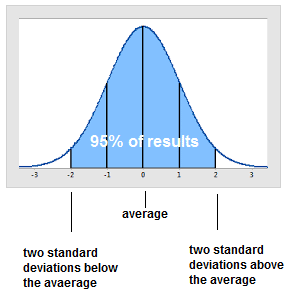
This is the normal distribution curve. 95% percent of people will fall within two standard deviations from average (the area coloured blue).
So if you are especially tall, especially short or especially muscular you may find you don’t benefit as much from using the quickest, easiest, least invasive, cheapest method of figuring out if you have obesity – calculating your BMI.
Fortunately for this segment of the population there are other methods available, such as waist-hip ratio (find out how to calculate it here), waist-height ratio, skin callipers, body composition scales and other specialised equipment.
The interesting thing about BMI is that contrary to popular opinion, studies show that BMI more often underestimates body fat rather than overestimates it.
People with a BMI of 25-30 fall in the overweight category. However, these large, multiethnic studies of men and women of all ages show that when percentage body fat is measured, over half of the people in this category actually have obesity. So BMI may miss people who appear mildly overweight but actually carry a lot of body fat. For these people, having a BMI outside the healthy range can be a call to action to focus on reducing body fat and a non-threating indicator that they may benefit from further assessment and treatment to improve their health.
Take home message:
BMI is not used because it is perfect or the most accurate measurement for every person in the population. BMI is not a diagnostic tool.
BMI is a good starting point to identify people with obesity so they can be further assessed to determine if and how they would benefit from having their obesity treated.