Bariatric Surgery refers to a suite of surgical operations performed on the stomach and intestines that alter the way food is consumed and absorbed. These procedures assist individuals with a high Body Mass Index (BMI) to lose weight and resolve weight related medical conditions.
For the 5 million Australians with obesity (defined as a BMI above 30), weight loss can be a struggle. Studies consistently show that diet and exercise typically produce modest results, not the extreme weight loss people expect. Typically, supervised diet and exercise programs achieve 10 to 20% excess weight loss at 12 months, with most experiencing weight regain by 18 months.
The NHMRC guidelines for managing adults with obesity state “bariatric surgery is more effective in achieving weight loss in adults with obesity than non-surgical weight loss interventions.” Depending on the procedure, bariatric surgery typically achieves between 50 to 100% excess weight loss at 12 months with maximal weight loss typically achieved by 18 months.
It is important to note that research shows any bariatric surgery is more effective than none at achieving weight loss and health improvements. However, the best results occur when the surgeon tailors the treatment to the individual by selecting the procedure that provide maximal long term weight loss with minimal long-term risk for that patient’s specific circumstances.
What are the commonly performed bariatric surgery procedures?
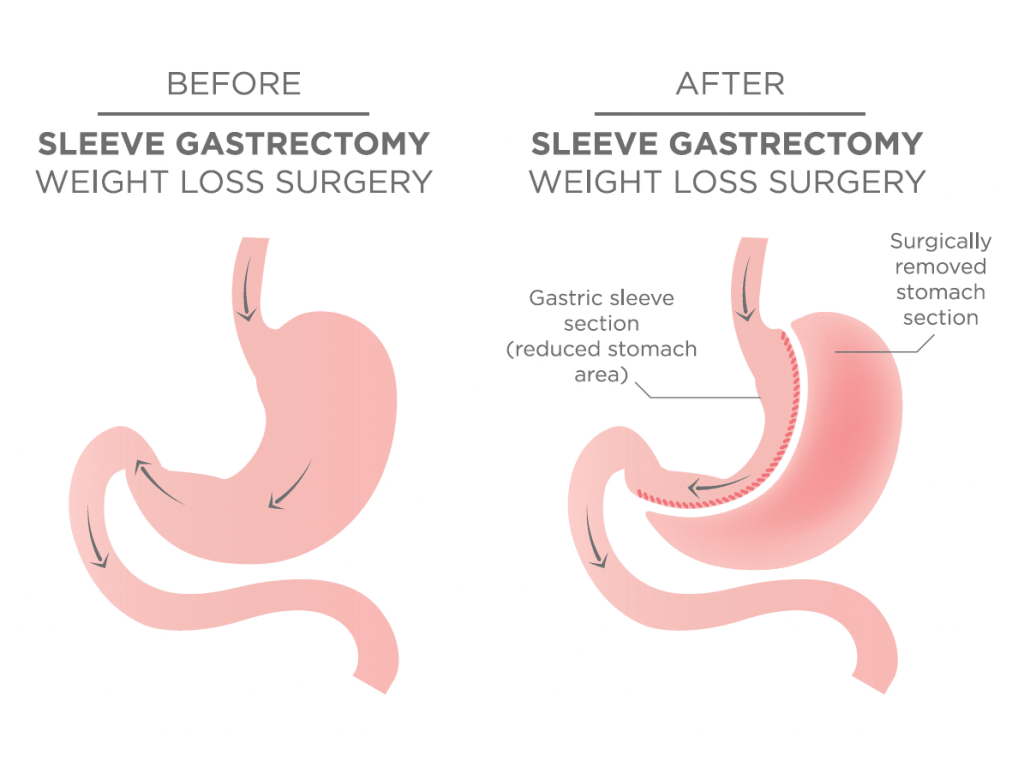
Laparoscopic Sleeve Gastrectomy
Also known as Vertical Sleeve Gastrectomy, during this operation a thin vertical sleeve of stomach is created using a stapling device. The resulting sleeve is about the size and shape of a banana. While the size of the stomach is reduced, the pylorus, duodenum and bowel remain unchanged.
The sleeve gastrectomy is the most commonly performed procedure in Australia as it typically provides 60-80% excess weight loss within 12 months, with a good eating quality of life and minimal risk of long term micronutrient deficiencies. It is viewed as a good primary procedure for the majority of people with obesity, accepting that like with hip and knee surgery, a portion of those may experience recurrence of their disease and benefit from revisional surgery in 5-10 years.
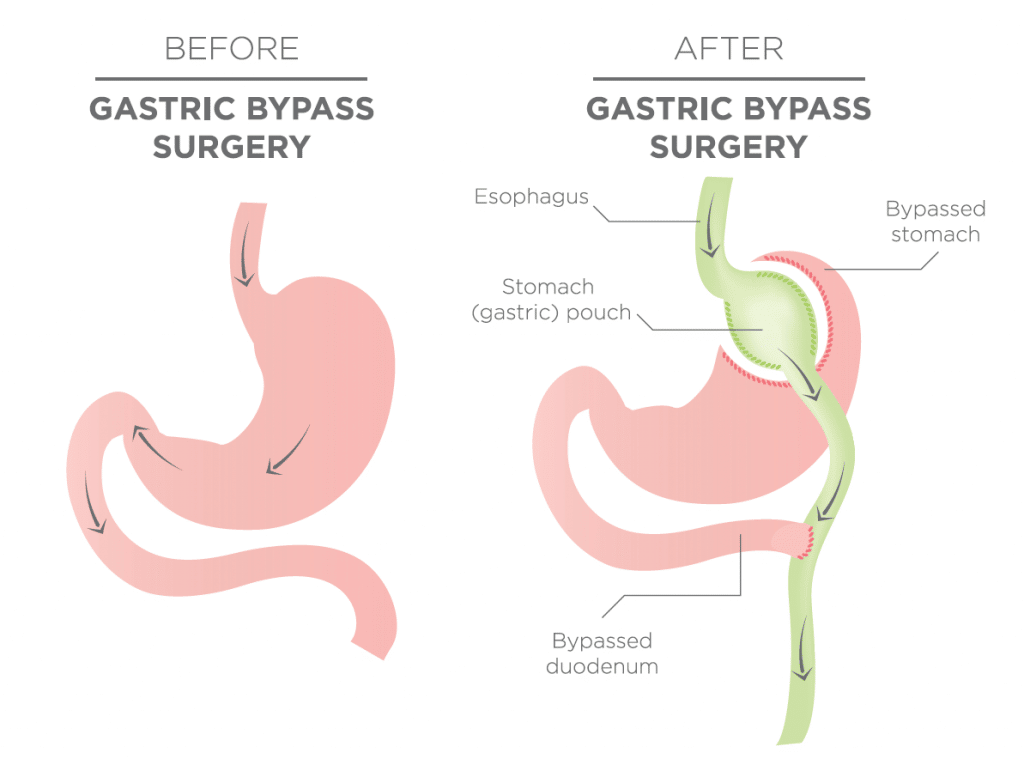
Historically, the classic Roux-enY gastric bypass has been considered the gold standard worldwide for weight loss surgery. A more recent modification has evolved called the single anastomosis gastric bypass, also known as the Omega loop or ‘Mini’ bypass, which also shows good results.
A gastric bypass both reduces the size of the stomach and bypasses part of the small bowel. During the laparoscopic procedure, a pouch of stomach is created with a stapling device, then connected to a lower section of the small bowel, bypassing approximately the first third of the small intestine. Gastric bypass typically produces greater sustained weight loss (60-85% excess weight loss within 12 months) and greater improvement in weight related health complications such as Type 2 Diabetes (80% remission rate) than a sleeve gastrectomy, at the expense of an increased risk of micronutrient deficiencies and food intolerances if patients are non-compliant with their prescribed dietary and vitamin recommendations.
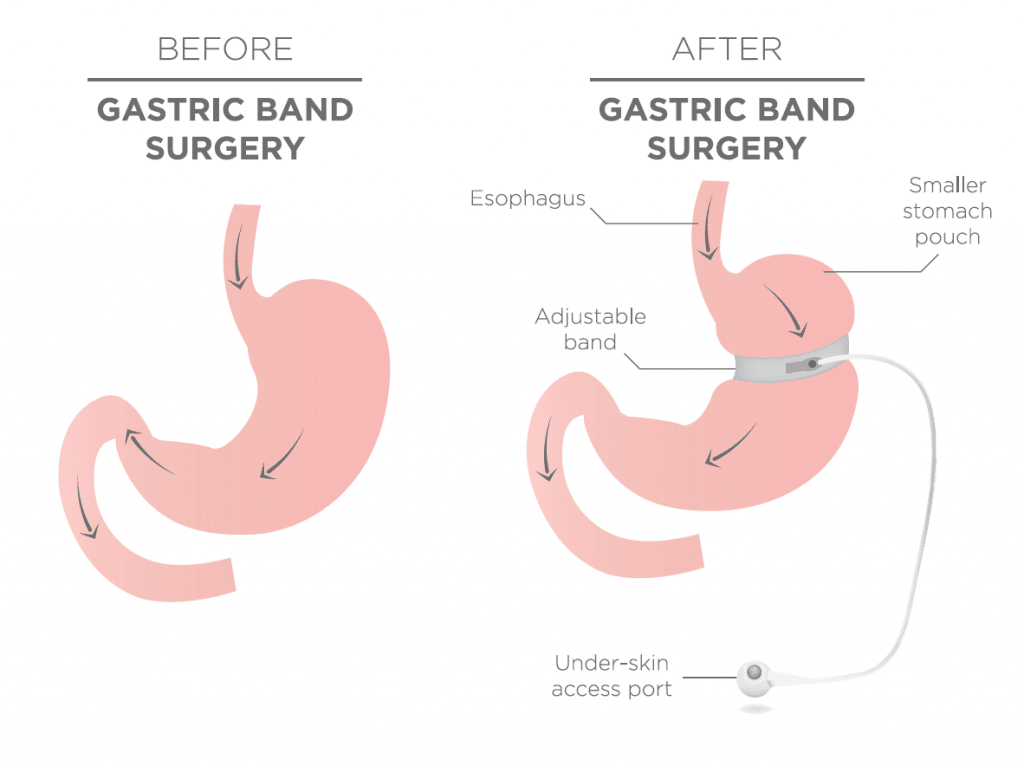
Laparoscopic Adjustable Gastric Banding
This laparoscopic procedure involves inserting an adjustable band around the top of the stomach to restrict capacity. The restriction can be increased every 2-4 weeks via an access port inserted just under the skin, until the optimal level is achieved.
Gastric band surgery requires a high degree of compliance to dietary and textural guidelines to prevent regurgitation, obstruction and band slippage. Weight loss is less predictable, typically achieving 40-50% excess weight loss, which is still significantly better than diet and exercise alone. It has the highest re-operation rate.
Laparoscopic SADI (Stomach Intestinal Pylorus-Sparing Surgery)
SADI is a promising weight loss surgery procedure that has evolved in recent years. SADI combines a sleeve gastrectomy with a “loop” small bowel bypass and importantly, retains the function of the pylorus as the outlet valve from the stomach. The initial published results show 90-100% excess weight loss at 12 months. It is anticipated that SADI will be more effective than a sleeve gastrectomy and will avoid most of the long term problems of both gastric bypass and duodenal switch surgery.
Who is a candidate for bariatric surgery?
NHMRC guidelines recommend bariatric surgery be considered for adults with a:
- BMI > 30 kg/m2 who have poorly controlled type 2 diabetes and are at increased cardiovascular risk
- BMI>35 kg/m2 and comorbidities that may improve with weight loss
- BMI > 40 kg/m2 regardless of their health
Take home message:
At the Surgical Weight Loss Centre we provide customised weight loss plans for each patient, delivered by a multidisciplinary team (including surgeons, dietitians, nurses, psychologists and physicians) with long-term follow-up.