Anybody who has ever tried to lose weight, especially a significant amount of weight, knows that it is like trying to swim upstream against a strong current. Even with a concentrated effort and absolute focus, it’s hard to make progress. If you let go and do nothing, you drift away.
So why is it so hard to meet our weight loss goals?
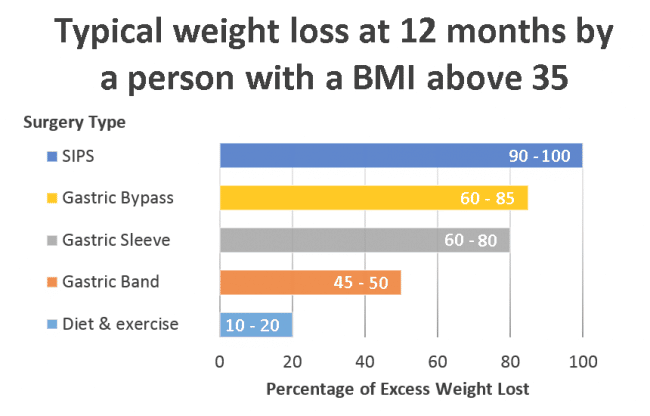
In part, it’s because of our expectations. The oft-recommended diet and exercise typically produces modest results, not the extreme weight loss people expect.
Medically speaking, the way to achieve successful sustained weight loss is to aim low and work hard. The Australian National Health and Medical Research Council’s (NHMRC) evidence-based guidelines for successful sustained weight loss advises to aim for a goal of 5-10% weight loss, achieved by a 2500 daily kilojoule deficit and five hours a week of moderate exercise. Progress should be monitored by a GP fortnightly for three months. If weight lost is less than 1%, the GP should arrange additional weight loss interventions.
For an Australian female of average height, the upper limit of the healthy weight range is 66kg, making a 5% weight loss of 3-4kg achievable with this recommended diet and exercise. But if you have 30-40kg to lose, like over 5 million other Australians, you have obesity and weight loss becomes more difficult.
It is important to understand that obesity is a chronic disease recognised by the World Health Organisation. It is not a sign of poor willpower or self-discipline. Obesity is a complex medical condition and the cause extends further than simplistic “calories in, calories out”. The interplay between humans and the environment, influenced by your genes, set the scene for your weight trajectory throughout life.
Body weight is regulated through a complex system involving the interaction between energy balance and feedback mechanisms that regulate a person’s appetite, energy intake and energy expenditure.
Appetite
Appetite is very hard to control. The biochemical pathways regulating appetite are powerful. It is believed that people with obesity, have a defective feedback control system where the appetite regulation part of the brain does not function properly, and instead, continues to stimulate hunger and food seeking behaviour, despite adequate energy reserves.
Calorie Absorption
It has been shown that those prone to obesity absorb more calories from their diet. This is affected by factors such as their gut flora (the micro-organisms found in a person’s gut) and their hormone response to food.
For example, a person who has ever had obesity typically requires 15% fewer calories to maintain an ideal body weight than someone of the same weight who has never had obesity.
Energy Expenditure
Activity and exercise account for only 20% of the energy a person expends. Almost 70% is expended through metabolic processes and another 10% through the thermic response to food. Energy expenditure varies between people. There is a strong relationship between resting energy expenditure and fat-free mass, which makes weight loss increasingly difficult for people with higher fat reserves. Studies have identified metabolically active tissues that decrease as a person’s body mass index (BMI) increases, which is one of the reasons obesity becomes self-perpetuating.
Excess fat reduces energy levels, making it more difficult to exercise. Intense or lengthier exercise causes the body to release the stress hormone cortisol which not only contributes to hunger, but also promotes fat storage independently of caloric intake. For men, extra belly fat also raises oestrogen levels and lowers testosterone, making it even harder to gain muscle and lose fat. Reduced muscle mass means a lower base rate of metabolism, increasing the ease of weight gain.
Fortunately, like many diseases, obesity can be treated.
The National Institutes of Health in America has recognised that weight loss surgery (also known as bariatric surgery), is the only effective long-term treatment for people with a BMI above 35. The NHMRC guidelines advise GPs to consider bariatric surgery for adults with a BMI above 35 who have obesity related health complications, and for all adults with a BMI above 40 regardless of their health.
Weight loss surgery is a tool that puts people with obesity back on an even playing field with everybody else. It allows their efforts toward weight management to be effectual and sustainable. Gastric sleeve and gastric bypass surgery typically produce sustained weight loss of between 60% to 80% of excess weight. For a female of average height with a BMI of 40, this would be about 24kg to 32kg, or about 35% of their initial body weight.
If you have obesity and have repeatedly found that diets don’t work for you, it is important to remember that you have not failed and that you are not a failure.
Like millions of Australians, you have a chronic disease that requires the appropriate treatment. Discuss with your doctor if, under the NHMRC guidelines, bariatric surgery would be an appropriate treatment for you.